Exclusive Breastfeeding: What to Know as a First-Timer
It will save us money, it is convenient, and it is the best for babies. These were and still are the reasons why I am into exclusive breastfeeding.
I was not breastfed as a baby. I asked my mom why and she recalled saying she seemed to have no milk.
Breastfeeding wasn’t as encouraged and recommended a few decades ago. Aside from information not easily available to new moms, doctors even used to prescribe formula. Now, many hospitals have no bottles allowed policy to give way to breastfeeding.
If you plan to exclusively breastfeed, read on to help get yourself ready.
What is Exclusive Breastfeeding?
Exclusive breastfeeding (EBF) is defined as giving your infant no other food or drink — not even water — except breast milk.
The World Health Organization (WHO) recommends mothers worldwide exclusively breastfeed infants for the first six months to achieve optimal growth, development, and health.
From the age of 6 months, children should begin eating safe and adequate complementary foods while continuing to breastfeed for up to 2 years and beyond.
Even though children would be eating solid food in their 6th month, breastfeeding mothers still use the term EBF if they are still not supplementing their babies with other milk.
Breastfeeding facts
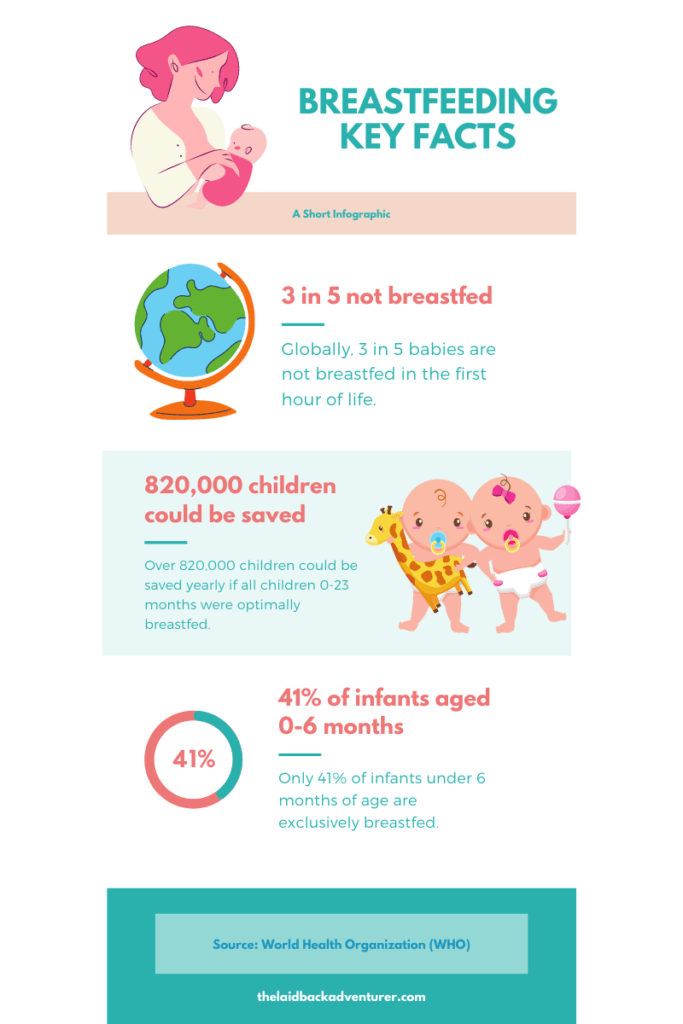
Breastfeeding from the first hour of birth
Unicef and WHO recommend that breastfeeding be initiated within an hour after birth. The immediate skin-to-skin contact between mom and baby has been shown to increase the chances that babies are breastfed. It also helps regulate a newborn’s body temperature and exposes them to beneficial bacteria from the mother’s skin.
As your baby tries to latch on, his suckling also stimulates your body to produce milk.
In other cases where the baby is unable to breastfeed directly (premature and in NICU) or the mom suffers from conditions that prevent her from nursing, moms can start to express milk.
Breast milk is even more critical to premature babies that when mom’s milk is unavailable, a donor’s breast milk is encouraged.
Many moms who weren’t able to feed directly from the breast at the start can still be successful in breastfeeding.
Breastfeeding after a c-section
Sadly, I wasn’t able to breastfeed during the magic hour. My baby and I barely had interaction right after birth. After he was pulled out, shown to me and they took pictures of us, I was out.
This is one of the reasons why I pout at the thought of my c-section. It felt like I was robbed of that unang yakap (first embrace). I was only able to breastfeed five or six hours after the surgery when I could finally manage to keep myself awake.
Mothers who deliver by C-section usually face multiple challenges after childbirth, like managing the effects of anesthesia, recovering from surgery, and finding help to hold the baby safely. But with the right support — training birth attendants, putting breastfeeding policies in maternal wards, and involving fathers in breastfeeding — most newborns delivered by C-section can be put to the breast within the first hour.
UNICEF
Nevertheless, I was able to exclusively breastfeed my son for the first six months (and counting).
Breastfeeding for the first time
It is normal for a first-time mom to have cracked and sore nipples in the beginning. Your boobs aren’t used to breastfeeding after all and don’t forget that even your baby isn’t used to nursing either.
However, take note that breastfeeding shouldn’t be painful in the long run. Your wounded nipple will heal and if everything is done right, you won’t dread nursing your newborn (until he’s teething).
It is crucial for your baby to have the correct latch. This way he will drain your boob efficiently and your breasts won’t likely suffer from clogged ducts and mastitis. Plus, your milk supply won’t dip down because the more your baby feeds, the more milk your body makes.
An incorrect latch can lead to your baby not being fed enough, having poor weight gain and being unable to reap all the benefits of your milk.
Like any other skill, it takes time, patience, and practice to get used to breastfeeding. You can always ask for help from your healthcare providers if you are not sure whether you are nursing your newborn right.
How much and how often should I breastfeed?
“Responsive feeding” or breastfeeding on demand is offering breast milk whenever your baby is hungry, as often as he wants and as long as he likes.
Even though every baby is different, a newborn usually breastfeeds every 2-3 hours. Breastfeeding sessions may take 20 up to 30 minutes on each breast. A rough guide is you’ll be feeding your infant at least 8 times in 24 hours.
Don’t worry about breastfeeding often as it won’t spoil your baby. In fact, attending to his needs sooner not only makes his tummy full, but also makes him feel secure, and contributes to his development.
It is wise to be familiar with hunger cues such as lip-smacking and thumb sucking. Don’t wait until your baby is crying before you feed him. Crying is a late sign of hunger.
Breastfeeding master class from UNICEF
Watch this 3-minute mini parenting master class as lactation expert Dr. Michele Griswold answers some of the most common breastfeeding questions (like should I wash my nipples before breastfeeding?).
Will you make enough milk?
Your milk will be in small amounts at first. Your supply also adjusts to how much your baby needs and depends on how often you feed him. But since we can’t measure how much milk goes to our babies’ stomachs, many new moms (me included) worry whether babies really are being fed.
That said, here are signs that your baby is having enough of what he needs:
Try not to stress and worry because it can affect your milk supply. Remember that hunger isn’t always the reason why an infant is crying.
Breast milk stages
It still amazes me how a mom’s body is enough (for the first six months) to provide the best food for her baby. Even more impressive is that breast milk composition changes over time to meet your feeder’s needs.
For the first few days after giving birth, you will produce the early milk Colostrum. Also called ‘liquid gold’ because of its yellowish color, this milk is said to be the richest in nutrients. It also protects your baby’s gut from germs and inflammation by coating its lining.
After the colostrum comes the Transition Milk, which is higher in fat, calories, and lactose to aid your rapidly growing newborn.
By week 4 and onwards, your body will be producing the Mature Milk that’s rich in protein, sugar, vitamins and minerals, and other components to support your baby’s growth and development. You would want to read Medela’s article on what’s in your breast milk and be mindblown with how brilliant human milk is.
Still, breastfeeding is a personal choice. If you are on the fence or you want to have an idea of how similar breast milk is to infant formula, you can read it here.
What are the health benefits of breast milk?
“Breast milk is best for babies up to 2 years.” We’ve heard and read it again and again. What does it really mean anyway?
For babies
Being exclusively breastfed for the first six months reduces their chances of developing health problems such as:
- Ear infections
- Bacterial meningitis
- Gastroenteritis
- Urinary infections
- Respiratory infections
- Diarrhea
- Allergies and Eczema
- Diabetes
- Childhood cancers such as leukemia and lymphomas
- Less likely to be a victim of sudden infant death syndrome (SIDS).
Breastfeeding when your baby is sick is even more beneficial as of lactation and breastfeeding expert, the late Professor Peter Hartmann.
When breastfed babies get sick, their mothers’ bodies will produce specific antibodies against the infection their babies picked up. Breast milk isn’t just food; it is also protection and medicine for your baby. Who wouldn’t want a boost in immunity, right?
Nursing your newborn also helps him sleep. Suckling is soothing and calming to babies that most just sleep after a feed. Get ready to feel like a human pacifier (consider it a superpower).
For mothers
Moms also obtain physical, emotional and mental benefits from breastfeeding their babies. It reduces their risks of breast cancer and ovarian cancer. It also lowers their lifelong risk of heart disease and type 2 diabetes.
Breastfeeding releases oxytocin or the “love hormone” that helps make your uterus contract, making it shrink faster to its normal size. And speaking of oxytocin, a study found that mothers who have higher levels of this hormone had fewer anxiety and depression symptoms.
Aside from those above, breastfeeding benefits moms by:
- Having less postpartum bleeding (because of the uterine contractions)
- Increased confidence and self-esteem
- Having unique bonding time with baby
Since breastfeeding uses energy and burns extra calories, you will likely return to your pre-baby weight sooner. I am breastfeeding for more than a year now and I am below my pre-baby weight.
Okay, I know it’s not set in stone and many moms said they still gain weight even though they are exclusively breastfeeding. There really are other factors such as your weight before you got pregnant, how much your current food intake is, and what kind of lifestyle you are used to having.
If you are breastfeeding, you save money (unless you can’t keep still when it comes to nursing accessories). It is also convenient especially when you travel with your little one. Just whip out your built-in milk machine and that’s it. Your milk is always clean and at the right temperature. No need to bring (and wash) cans and bottles and teats. You are helping the environment too!
Is exclusive breastfeeding tiring?
YES! At first!
To my surprise, exclusive breastfeeding during the early weeks is exhausting. It doesn’t look like an activity that will wear you out but milk production takes energy and your body has already gone through so much.
Excluding what’s happening with your boobs, moms usually are hungry, thirsty, sleep-deprived, and have no time for themselves.
On the bright side, breastfeeding will get easier as your body and lifestyle adjust. Even though I was tired, I felt like a queen with a superpower just because I’m using my milk bar.
If you want to feel inspired and motivated to continue breastfeeding exclusively, think of the seemingly endless benefits of your baby consuming breast milk. You may also try to compute how much you are saving because you’re nursing.
Common breastfeeding problems and solutions
Is breastfeeding easy? Well, not if you have these challenges below.
- Incorrect latch. Your baby should be sucking not just the nipple but the areola. Don’t settle on having a poor attachment as it could lead to a lot of other breastfeeding struggles.
- Cracked nipple. Another cool thing about breast milk is that it can treat cuts and scrapes because of its antibacterial property. You may also opt for nipple soothing salves.
- Engorgement. Breast engorgement is very common during the early days postpartum as your milk starts to come in. You can express milk to help with the fullness, especially if your baby seems to drown from your milk while he’s nursing. Here are also other ways to remedy discomfort from engorgement.
- Leaky breasts. Just the thought of your baby can trigger milk letdowns. You may use breast pads to avoid getting your shirt stained. When you’re nursing, use a milk catcher on your other boob and have the milk for later use.
- Blocked milk ducts. Have a warm compress and massage your breasts. Try to break the lumps of milk so the next time your baby latches on, he can drain your boob effectively.
- Mastitis. Swollen, red, and painful lump on your breast. I thought I won’t ever experience this. The infection made me feverish and for some reason, moving my body hurt. It seemed as if my whole body was connected to the achy boob. I was given antibiotics and pain relievers to treat this. The good news is you can continue breastfeeding even if you have mastitis.
- Low supply. Keep breastfeeding. The supply of milk will take its cue from the demand of baby nursing. You may also take lactation supplements.
Support system during your breastfeeding journey
Unicef and WHO launched the Baby-Friendly Hospital Initiative to encourage hospitals, birthing centers, healthcare workers, government and families worldwide to better support early and exclusive breastfeeding.
The drive includes ensuring that healthcare staff has sufficient knowledge, competence, and skills to support breastfeeding. They should also facilitate immediate and uninterrupted skin-to-skin contact and support mothers to initiate breastfeeding as soon as possible after birth.
Lactation Consultants
For those who need help at some point, a lactation consultant can be a great guide to managing common breastfeeding difficulties. Even though I read a lot about breastfeeding when I was still pregnant, a hands-on and face-to-face discussion with a lactation nurse gave me everything I needed.
We were worried that our newborn wasn’t getting any milk since he was crying a lot (it seems to us, new parents). Thankfully, the hospital has a lactation nurse. She gave me a lactation massage as well as tips on how to properly position my baby for a feeding session (football hold for a c-section mom).
I feel obliged to tell you that a lactation massage isn’t an enjoyable one when your boobs are full of milk and you have clogged ducts. Breaking down the lumps of milk through massage is actually painful.
Family and other breastfeeding mom (groups)
I am blessed to have support around me. Since it is hard to move around after a c-section, my main job during the first weeks was to keep the newborn fed. My husband, my mother, and even my sister-in-law took charge of the other demands such as changing diapers, burping, and rocking my son to sleep.
Talk to friends who had the chance to breastfeed. Online groups are also helpful. You will find that most moms are always ready to provide insight whether you are asking about breast pumps or tips to increase milk supply.
Remember that if your issue is medical-related, it is best to discuss it with your healthcare provider. Your doctor and your baby’s pediatrician can provide support. Baby tracking apps also provide ample information as guidance.
Employers
Breastfeeding shouldn’t stop just because you’re about to go back to the workforce. Employers play a role in helping mothers continue breastfeeding for as long as they choose.
The right to breastfeed in the workplace is critical to women who wish to continue breastfeeding their children, as are sufficient time and appropriate spaces for breastfeeding or expressing and storing breastmilk.
UNICEF
Pumping at work is normal. Many employers designate a room for a mom to express her milk and store it safely until she takes it back home. There are portable breast pumps that moms can bring to work. But the game-changer they say is a wearable breast pump.
Pumping when exclusively breastfeeding
Does pumping count as exclusively breastfeeding? If you pump, store your milk, and feed it to your baby using a bottle, it is still considered EBF.
Some reasons for this arrangement could be:
- You have a premature baby in the NICU who can’t breastfeed yet
- Your baby has difficulty latching on
- You want to know if you are producing milk (or how much you can)
- Breastfeeding is painful and you want a break
- You have twins or more
- You will go back to work outside your home
- You just want to make sure you have a stash of breast milk
- You don’t want to breastfeed
Many moms do bottle feeding as well as a direct latch. For example, you breastfeed at home whenever your baby needs it. When you’re away, your partner or a caregiver can offer your son a bottle from the pumped milk stash you built.
Pumping and storing breast milk in appropriate bags and then placing it in the freezer means you can use it later. This way, the dad can also bond with the baby during his feeding duty.
Try to delay the use of bottles and pacifiers as they could get in the way of the baby’s ability to latch on to the breast. If you can, wait at least 3-4 weeks before offering the binky.
Exclusive Pumping
Exclusive Pumping or EPing is just how it sounds. It is breastfeeding without nursing.
Having breast milk in a bottle still makes for good food. However, this breast milk has lower benefits when it comes to immunity. When a baby latches on the breast, the mom’s body makes antibodies depending on what the baby needs that are detected through the baby’s saliva. So the absence of a direct latch means breast milk won’t be as custom-made.
Storing and donating breast milk
After expressing or pumping your breast milk, the proper way of storing ensures its safety and quality. The Centers for Disease Control and Prevention (CDC) has these guidelines for the proper storage of human milk.
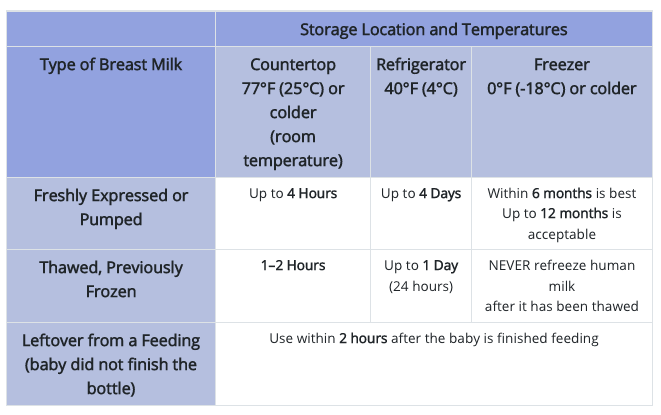
You can also access and download their pdf guide for more information on the storage and preparation of breast milk.
Not all moms are able to breastfeed. Some women have health conditions that inhibit them from producing enough milk. If you are pumping to build a stash or has an oversupply, I hope you consider donating breast milk.
I used to think it was silly to save and store milk for others, only because I thought no one would need it. But having been to online breastfeeding groups, I learned that plenty of mothers are hoping to receive human milk donations. The number of babies in need (sick babies mostly) is saddening. When I get pregnant again I’ll be sure to donate more.
Extended breastfeeding
While exclusively breastfeeding your baby for the first six months is what is recommended, many moms continue until toddler age.
WHO recommends that infants start receiving complementary foods in addition to breast milk when they reach 6 months. Extended breastfeeding is when you continue offering breast milk past the age of 1.
Breastmilk provides all the energy and nutrients that the infant needs for the first months of life, and it continues to provide up to half or more of a child’s nutritional needs during the second half of the first year, and up to one third during the second year of life.
WHO
Ultimately, it’s up to you when you’d want to stop breastfeeding. Over time, the primary source of nutrition for your little one will become the solid food they take.
Why do moms stop breastfeeding early?
Whether the baby decided he’s had enough of the breast or the mom has reasons why she has to wean the tot, stopping breastfeeding is influenced by many factors.
Some reasons can include:
- Issues with lactation and latching
- Returning to work (with unsupportive work policies and parental leave)
- Medical reasons or taking medications
- Concerns about infant nutrition and weight (they will resort to formula)
- You reached your target months or age to breastfeed
- You are pregnant and are feeling uncomfortable with nursing
- Cultural norms and lack of family support
Weaning from breastfeeding
Weaning from your breast is best done gradually. Whether you would like to switch to formula or do mix feeding or you’re done, dropping 1 or 2 feeds per day will slowly decrease your milk supply. It will make you less likely to suffer from clogged ducts or mastitis.
For whatever good reason you have for weaning, try to take it slow. It could be hard for your little one especially when he’s exclusively breastfed.
However, some babies or toddlers suddenly decide they’re done. Some though just want a break. Whether the change is initiated by you or abruptly decided by your tot, you are bound to feel some sadness. Breastfeeding is a bond after all.
Tips for exclusively breastfeeding moms
While still pregnant
After giving birth and still at the hospital
When at home
As much as possible, try delaying giving your baby a bottle or a pacifier until breastfeeding is established. Some babies love the easier milk flow from a bottle they develop nipple preferences.
The importance of breastfeeding is unparalleled — this one we cannot argue. Many mothers suffer from guilt for not being able to breastfeed their babies. On the other hand, some moms had no plans to breastfeed from the beginning and go formula right from the start.
The best choice is what works for you and your family. Many factors affect a mom’s decision to nurse and I found that you should never judge or even think that you are doing better than anyone else.
We all want babies to receive the best care available and mothers are all surely working for it.